What is peripheral arterial disease, symptoms and diagnosis?
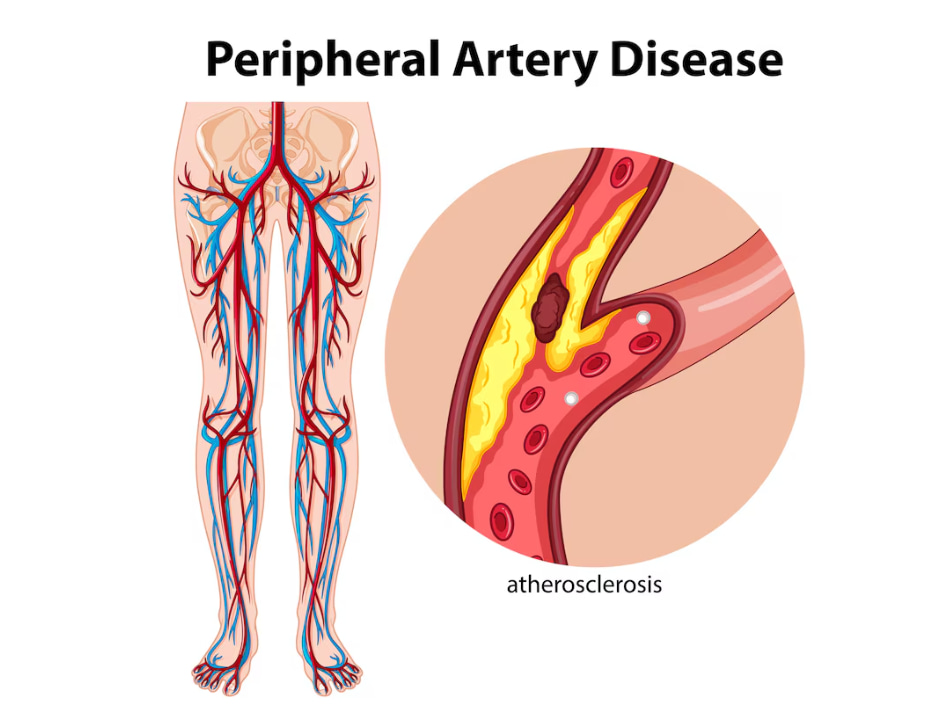
Symptoms include:
1. Leg pain or cramping (intermittent claudication) when walking or exercising
2. Weak or tired legs
3. Foot or toe pain at rest
4. Coldness in the legs or feet
5. Sores or wounds on the legs or feet that won’t heal
6. Pale or blue-tinged skin
7. Decreased hair growth on the legs
Diagnosis involves:
1. Medical history and physical exam
2. Ankle-brachial index (ABI): compares blood pressure in ankles and arms using a vascular Doppler
3. Toe- brachial index (TBI) using a PPG sensor
3. Doppler ultrasound: measures blood flow
4. Angiography: X-rays or CT scans with contrast to visualize arteries
Early detection and treatment of diabetic neuropathy are crucial in managing symptoms and preventing further complications. By addressing the condition promptly, individuals can improve their quality of life, maintain mobility, and significantly reduce the risk of severe outcomes like heart attacks, strokes, and amputations associated with advanced nerve damage.
What is diabetic neuropathy and what are the simple tests and devices used to detect?

There are four main types of diabetic neuropathy:
1. Peripheral neuropathy (most common): affects nerves in the legs, feet, arms, and hands
2. Autonomic neuropathy: affects nerves controlling involuntary functions like heart rate, digestion, and blood pressure
3. Proximal neuropathy: affects nerves in the thighs, hips, and buttocks
4. Focal neuropathy: affects specific nerves, causing pain, weakness, or numbness in a limited area
Symptoms:
1. Numbness, tingling, or burning sensations in the feet, legs, hands, or arms
2. Pain or discomfort, often worse at night
3. Weakness or fatigue in the affected limbs
4. Loss of reflexes
5. Difficulty with balance or coordination
6. Digestive issues, such as nausea, vomiting, or diarrhea (autonomic neuropathy)
7. Dizziness or lightheadedness (autonomic neuropathy)
Tests and Devices:
1. Monofilament 10gm Test: A thin, flexible fiber is pressed against the skin to assess sensitivity. If the patient can’t feel the filament, it may indicate nerve damage.
2. Tuning Fork Test: Vibrations from a tuning fork are placed on the skin to evaluate sensation. If the patient can’t feel the vibrations, it may indicate nerve damage.
3. Pinprick Test: A small needle is used to assess pain perception. If the patient can’t feel the pinprick, it may indicate nerve damage.
4. Biothesiometer – Vibration Perception Threshold (VPT) Testing: A device measures sensitivity to vibrations. If the patient can’t feel the vibrations, it may indicate nerve damage. These devices have computer connectivity for storage and reporting.
5. Nerve Conduction Studies (NCS): Measures nerve signal speed and strength. It can help diagnose and monitor neuropathy progression.
6. Thermometry HCP: Thermal perception threshold ( Hot and Cold): A device measures sensitivity to temperature. If the patient can’t feel the thermal changes (cold and hot), it may indicate small nerve damage.
These tests are simple, non-invasive, and can be performed in a healthcare provider’s office. They help diagnose diabetic neuropathy, monitor its progression, and guide treatment decisions.